
Tim Russert: Dead at 58
I was shaken by Tim Russert's death from a heart attack at age 58 on June 13, 2008. As one of NBC's top newscasters, he was beloved by millions of Americans who would watch him each week on Meet the Press , as he unrelentingly asked the tough questions to our politicians.
When men (and less frequently women) die suddenly in middle-age it's almost always caused by coronary artery thrombosis, a blood clot suddenly forming in one of the two arteries supplying the heart muscle itself.
Although the heart pumps all five liters of your blood every minute, it itself gets its oxygen and nutrients only from the blood supplied by the 4 mm diameter right and left coronary arteries that run on its surface, starting from the aorta.
Heart attack caused by coronary artery disease is the number one killer in the United States and Western Europe. It causes over half a million deaths (USA) per year. Stroke is the second most common cause of death, and it occurs by exactly the same process, obstruction of the arteries to the brain.
Heart attacks occur when a coronary artery suddenly plugs up. Here's how it happens.
Over decades plaque builds up on the sides of the arteries. Plaque starts out as fat deposits in the internal wall of the coronary arteries. After many years that fat becomes calcified and stoney hard.
Heart attacks happen when a plaque ruptures, lifting off the wall of the artery, and precipitating a blood clot that completely plugs it. The heart muscle then has no blood supply and dies. If the heart can't pump blood, then the patient dies as well. (This is a simplification, but it'll do for now.)
As an ER physician I have, of course, taken care of hundreds of patients with hearts attacks. We see them everyday. However, my involvement with heart attack also has a personal angle.
Arteriosclerosis (Latin for hardening of the arteries) killed my grandfather in middle age. Arteriosclerosis killed my father, and, as a young physician, I watched that process unfold in him. It started with angina in his fifties, heart attacks in his sixties, and strokes and death in his seventies. I helped wheel him into the operating room when a leg was amputated for clogging of the arteries in his legs.
Armed with my knowledge of medicine and having watched my father's tragic disease, I've striven all my adult life to avoid arterial disease and its attendant ravages.
I've always been athletic — tennis in high school, running three miles a day from age 18 to age 33, vigorous hiking and cycling during the past thirty years. With all that physical activity I've always assumed that I myself would never get atherosclerosis.
My cholesterol scores were, I thought, reasonably ok — about 230 or so in my forties and early fifties — (what constitutes normal has steadily decreased in the past twenty years.) And, I started taking statins about a decade ago with a resulting total cholesterol of about 150, LDL cholesterol of perhaps 80 or below, and HDL cholesterol of 42 (not great).
I've never smoked — don't ask me about med school at UCSF in the late sixties in the Haight-Ashbury — and my blood pressure's been normal.
Given all that, it was quite a shock to find that, in fact, I have arteriosclerosis . In another essay I'll talk about what might've gone wrong.
Our subject today is how I found out.
First, I must say I've never had any symptoms of narrowed arteries.
I hiked 14,500 foot Mount Whitney a decade ago, and every year I used to climb Half Dome in Yosemite with my son. I still regularly hike a local 2,000 foot mountain So, no symptoms but ...
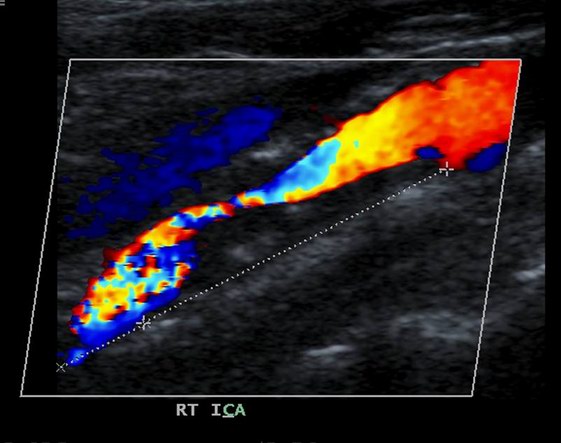
A lengthwise cross-section of a patient's (not mine) right internal carotid artery. Blood is flowing from the upper right to the lower left. It's flowing around a large (black) obstructing plaque. The speckled colors at the lower left are caused by post-obstructive turbulent flow.
Wake Up Call #1 : My Carotid Ultrasound
Before I retired from practice, we ER docs at Kaiser were learning to do bedside ultrasounds. Ultrasound is now a regular part of the ER armamentarium. We mainly use it to diagnose problems related to early pregnancy like miscarriage or tubal pregnancies.
At the end of our teaching session, driven by curiosity, I asked our instructor to scan my carotid arteries. The carotids take off directly from the aorta, and they are an easily accessible place (in the neck) to determine the state of your arteries. As the carotids go, so go the coronaries.
The exam takes just a few minutes and involves nothing more than the tech's moving a probe around on your neck.
When my left carotid was being scanned, one of my colleagues gasped and said "what the hell is that?" I thought my colleague was just joking at my expense; however, the teacher said they were seeing an irregular calcified plaque. In one view it looked like an iceberg; however, in the transverse cross-section it appeared it was in actuality only about a twenty percent obstruction.
The next day I had a a formal ultrasound (larger, higher resolution machine) that confirmed this finding and, furthermore, showed that my flow velocities were all normal.
With significant obstruction the blood flow speeds up. Picture what happens when you partially obstruct the end of a running garden hose with your thumb — the water then jets out. If the flow velocities are normal, then the obstruction is not significant.
When we're young we think we're going to live forever. This was particularly true for me, because I'm extremely health conscious and would, in fact, love to live forever. Nothing thrills me as much as watching the future unfold.
Unfortunately, that little episode brought my notion of living forever unscathed by time to an abrupt halt. I WAS MORTAL! #$%^*! I was going to die of the same disease that killed my father and grandfather.
I increased my dose of statins, was somewhat more assiduous about my diet and exercise, and I comforted myself with the notion that twenty percent obstruction wasn't all that bad. Also,it seemed likely that that calcified plaque had probably been growing for decades and wasn't likely to go anywhere. (This has proven to be the case. I've had a few ultrasounds since then and there has not been any progression.)
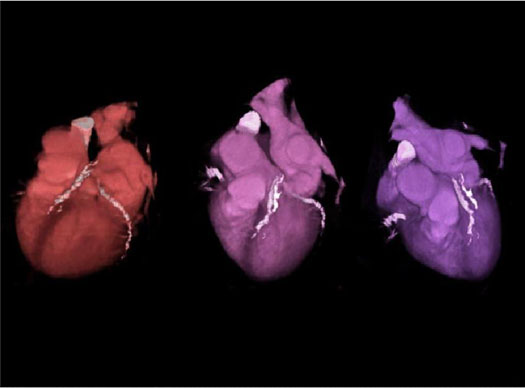
A coronary artery calcium score or CAC is done by ultrafast CT in one breath hold. The CT is synchronized to your electrocardiogram, and its purpose is to image calcified plaques (if any) in your coronary arteries. (There should be none.)
Nowadays this test is usually done with a 64-slice CT scanner, but the test has been available with ultrafast e-beam CT scanners for about two decades.
By the way, this is completely non-invasive: not even an IV is required. Don't confuse this with a coronary arteriogram, which is highly invasive.
I need to mention that the CAC like any CT scan incurs a lot of radiation exposure . It's many times the radiation from a typical chest x-ray.
The information gained may outweigh the risk. But, this is definitely an issue that must be weighed and discussed with your physician.
A good friend of mine’s dad had a coronary CT scan about two decades ago. The dad, who was energetic, delightful, and a well-known local citizen, had arteriosclerosis on his CT that was practically off the scale. Despite this, he was completely free of symptoms (taking BP meds, but not on statins). Ignoring the scan, he continued to live the life of a gourmet/gourmand and died suddenly of a heart attack about three years later in his early sixties. (His son, sensitized to the risk factors, began statin therapy soon thereafter.)
The test cost me about $300, may not be covered by insurance, and is definitely not a routine part of any internist's screening exams (like an ECG or chest x-ray, or lipid panel.) Given those barriers, I myself did not get the test until a decade ago.
Stupid me! My carotid ultrasound should have motivated me. I was persuaded ultimately by a discussion in Fantastic Voyage, the health book by Ray Kurzweil and Terry Grossman. To get the test I had to go outside of Kaiser, my insurer. (Kaiser's policy, in common with many other institutions, is that the test provides no new actionable information that can't be gotten by other means. I vehemently disagree and present the case for a coronary calcium scan below.)
My test was rapidly completed and, full of optimism, I cheerfully asked the CT tech "well, am I going to live?" The tech, not full of optimism, muttered, "it's always the doctors and nurses." Suddenly, feeling a lot less cocky, I asked "what's going on?"
As I reviewed my scan with him, it was obvious that my cardiac scan was not ok. There were obvious calcified plaques and my total calcium score was above normal for a man my age. Somehow all my running, hiking, biking, and clean living hadn't worked!
What had gone wrong? If a conscientious, physically fit physician couldn't prevent hardening of the arteries then what hope could there possibly be for unmotivated civilians?
This also motivated my writing on Optimal Nutrtion and on Synthetic Coronary Grafts.
I'm writing this essay now to give you help you may not get from your family physician or internist.
Most health plans and insurance companies won't pay for coronary calcium scans and the indications for a carotid ultrasound are also quite limited. These tests, however, changed my life and provided information I absolutely needed to know.
There are two issues. 1) Do the tests provide information that's not available from cheaper blood tests?
2) Suppose your ultrasound or CT shows calcified plaques. Can you do anything about it?
Do the imaging tests provide new information? Absolutely! While it's clearly important to measure your blood pressure, cholesterol (total, LDL, HDL) and triglycerides those are indirect influences on the amount of plaque in your coronaries and carotids. What really counts is what is actually there. Why guess or use indirect measures when the radiologists or ultrasonographers can actually see it.
The x-ray exposure is a real safety concern, as I mentioned above, and is particularly an issue when contemplating serial CT's over time. (This is not an issue with ultrasound.)
Now, suppose the imaging tests show plaque build-up. Can you do anything about it? Absolutely!
This means your interventions need to be persistent and aggressive — maximizing calorie restriction and weight loss, optimizing diet (mainly vegetarian), optimizing exercise, and probably taking statins. For many people these are huge, life style changing interventions that they wouldn't undertake without these scans.
The issue of whether atherosclerosis is reversible warrants a major discussion. Here, suffice it to say that the answer is a qualified "yes!"
Cardiologists divide plaque into two categories: calcified plaque and vulnerable plaque. The calcified plaque is like a statue. It's hard as bone (it is bone!) and removing it requires a rotary instrument like a dentist's drill. The good news is that, like a statue, it's not going anywhere.
Vulnerable plaque, on the other hand, is soft, lipid-filled plaque that can accumulate and change shape in a matter of days. This is the type of plaque that medical scientists have implicated as a major cause of heart attacks and stroke. Vulnerable plaque can be abruptly lifted up by the blood stream and cause a sudden blockage of the artery. Fortunately, vulnerable plaque appears to be susceptible to reversal by statin drugs and by diet. Vulnerable plaque can be directly seen by intravascular ultrasound (IVUS) — a highly invasive test.
Shrinking of vulnerable plaque by statins has repeatedly been demonstrated by Steve Nissen, Chief of Cardiology at the Cleveland Clinic.
Also, Dr. Dean Ornish’s studies have shown reversal of vulnerable plaque by highly restrictive low-fat diets.
Although the ultrasound and the CT only detect calcified plaque, that is highly correlated with vulnerable plaque. Therefore, the presence of calcifications is a major tip-off that vulnerable plaque is also present.
When vulnerable plaque is present over time it gradually becomes calcified. While this narrows the artery, it may possibly decrease the chance of plaque rupture.
After years of studying the role of the CAC (the Coronary Artery Calcium score derived from CT), the American Heart Association (AHA) issued a definitive statement in 2007.
The majority of published studies reported that the "total coronary calcium score predicts coronary disease beyond standard risk factors.”
And the AHA’s final conclusion was this. "In intermediate-risk patients, it may be reasonable to measure the atherosclerotic burden using EBCT (e-beam CT) to refine clinical risk prediction and to select patients for more aggressive target values for lipid-lowering therapies. "
(Here the AHA was trying to be very conservative in their recommendation, lest they saddle the nation's health plans with unnecessary expenses (and patients with radiation.)
I think their conclusion is quite reasonable, if conservative. If your risk of heart disease is quite low — a woman under 55 or a man under 45 with no other risk factors — then the CT may be a waste of money and a needless exposure to x-rays.
Similarly, if you have multiple risk factors and are in the highest risk group, then again, the scan may be a waste of money, since you need aggressive intervention no matter what the test shows.
On the other hand, for the quite large subset in the intermediate risk category the scan may provide essential new information that can make a huge difference in treatment, life style, and outcome.
For those in the intermediate risk category, starting with a carotid ultrasound as I did, also seems like a reasonable way to go. Family physicians and internists may be more amenable to ordering a sono for you.
I did not discuss the various treadmill tests in this brief presentation. They're an important part of the work up of obstructive coronary disease and particulary in working up chest pain. Unfortunately, every ER physician has seen patients with heart attacks whose treadmill tests had been normal.
Health Care Disclaimer: I try to provide vital information of public interest. But, do not base any health care decisions on this.
Health care decisions depend crucially on your unique situation and can only be evaluated by your physicians. While I strive to provide accurate information, I can't guarantee its accuracy or completeness. All data, information, and medical consensus are subject to change without notice. I (Robert Blum, MD, PhD) accept no liability for the use or accuracy of this information nor any obligation to keep it current.